
Since the start of this decade, the healthcare sector has undergone major transformations, reaching new maturity levels in areas like telehealth, big data analytics, and AI adoption to an extent. Although adoption levels have been largely uneven.
Healthcare leaders have also faced the ‘perfect storm’ of challenges — the global pandemic, mass staff shortages, patient and practitioner demographics shifts, and ongoing cost squeezes. In such an uncertain climate, it may be hard to determine which areas deserve further attention (and financing) as the ROI of novel technologies isn’t always evident.
This post highlights the technology areas where digital transformation in healthcare will have the most impact in the next two to five years.
Four Technology Themes Shaping the Next Decade of Healthcare
As healthcare systems face staffing shortages, rising costs, and growing patient demands, leaders are increasingly turning to innovative technologies to improve service accessibility, diagnostic accuracy, and overall patient engagement.
Based on our analysis, four main technology themes will shape the future of healthcare: greater adoption of clinical decision support systems, remote patient solutions, increased focus on senior care technologies, and greater integration of AI into workflows.
1. Clinical Decision Support Systems
Clinical staff is at a tipping point: 53% of physicians report burnout. Emergency medicine (65%) and internal medicine (60%) specialists are even more stressed.
Prolonged stress and burnout drive the intention to quit, which has hardly abated after the pandemic. The World Health Organization (WHO) warned that European and Central Asian healthcare systems face a “ticking time bomb” — a combination of low pay, long hours, inadequate support, and serious staff shortages that can paralyze local healthcare systems unless diffused.
In the US, similar issues persist. Mercer estimates a shortage of over 100,000 healthcare workers by 2028. In Canada, the healthcare sector already had 96,200 vacant medical positions as of Q4 2022.
While healthcare staff shortages are a complex problem requiring multi-level intervention, one aspect can be swiftly addressed with technologies: physicians’ day-to-day well-being and productivity. In Europe, the ‘physician tools’ startup segment is worth over $25 billion, according to Dealroom. In 2022, these companies raised an extra $1.2 billion, despite the general dip in investments.
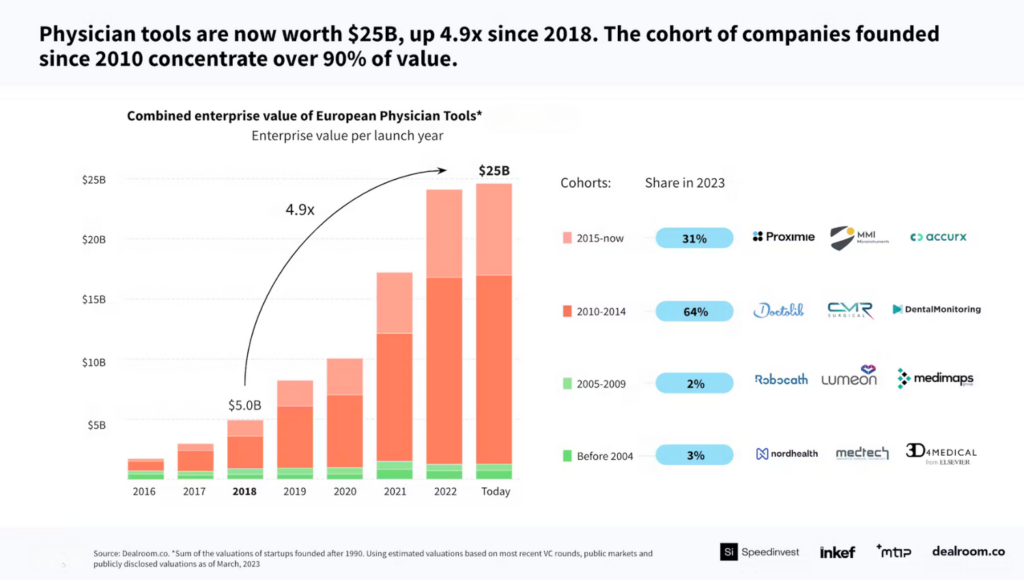
Source: Dealroom
Clinical decision support systems (CDSS) are a particularly promising market, expected to be worth $3.76 billion by 2031.
A CDSS is a collection of digital tools for streamlined information lookup, summarization, and analysis for diagnostic support. Advanced systems, powered by big data analytics, may include features like automatic cross-check of drug-disease interactions, individualized dosing support, or symptoms cross-validation across available order sets.
Epic Systems allows clinicians to use real-world data about similar patients for smarter care decisions. The Best Care tool compares the patient’s symptoms against the internal research database to identify similar cases. It offers contextual recommendations on effective treatments and connects the physician with a peer for a quick consult.
French MyPL, in turn, provides clinically validated patient information to oncology professionals. The web app offers access to the latest patient insights through convenient profiles, securely aggregated from EHR systems, PDF reports, and clinical notes. Each profile is compiled and validated by the company’s proprietary machine learning algorithms. Decision support is just one of the many viable use cases of big data analytics in healthcare.
Clinical decision support systems can also eliminate redundant steps and inefficiencies in healthcare delivery processes. Epic software helped several infusion centers optimize patient scheduling based on historical data and predictive insights, recommending the least busy days. Participating institutions managed to improve patient volume by 20%, increase gross income by 15%, and reduce wait times by 41%, according to a case study.
According to the American Medical Association, an average physician uses 3.8 digital tools. Adoption is increasing as three-quarters believe digital technologies can reduce stress and burnout.
2. Expansion of Remote Healthcare Ecosystem
Short-staffed healthcare practices have long waiting times for new patients, especially in countries with state-subsidized care. Other locations face increasing emergency admissions, prolonged stays due to complications, and a growing burden of chronic disease patients. Respectively, the adoption of remote patient management (RPM) solutions and telehealthcare systems ranks high on the leaders’ agenda.
Half of providers are either already offering RPM or plan to in the next year. And those who’ve already seen great outcomes from trials are expanding their programs to new specialties.
OptimizeHealth survey
Remote solutions for chronic disease management are in focus. Patients with chronic conditions struggle to receive timely care due to long waiting times and inertia to change. Digital technologies can help physicians better engage with chronic patients through timely remote interventions and digital therapeutics (DX) tools.
Fitterfly has created a diabetes-targeting digital program. The app compiles data from lab tests and the patient’s continuous glucose monitor (CGM) to provide tailored advice on diet, exercise, sleep, and stress management. Users can receive coaching or share their information with healthcare providers. Results from clinical trials show that after 90 days, 46.9% of participants reduced HbA1c levels by over 1%, and 38.5% achieved a weight loss of over 4%.
Other institutions are investing in digital front-door solutions — tools that ease access to healthcare services like online booking platforms, virtual queues, and on-demand telemedicine. These solutions can ensure a more even distribution of patients and workloads among professionals, leading to lower wait times and better overall access to healthcare.
Australia launched a national eHealth NSW platform, offering a unified online entry point to various digital health services. These include a Patient Reported Measures (PRMs) tool for sharing health outcomes and care experiences; a HOPE platform, and a Child Health Reminders (CHR) service for timely vaccinations.
Southern Cross Healthcare in New Zealand used a digital front door platform to improve the patient pre-admission process. Adopted in the Auckland Surgical Centre unit, the system allows 90% of patients to complete all necessary pre-admission and admission forms before the procedure. Clinical staff benefits from an 83% reduction in booking processing time per patient.
The trend we’re seeing is a progressive expansion of virtual hospital operations. Healthcare institutions further into their digital transformation journey are building fully digital units, offering on-demand online care and faster coordination to obtain physical admissions. Ksyos operates a national digital hospital in the Netherlands. Staffed with 7,500 general practitioners and 4,500 medical specialists and paramedics, the institution offers high-quality medical care without waiting times, digitally where possible, and physically where necessary.
Seha Virtual Hospital in Saudi Arabia offers 15 specialized health services, including psychiatry, kidney disease, diabetes, medical rehab, and genetic and geriatric diseases. It also provides virtual rays, e-pharmacy, and at-home care services. Digital at its core, Seha Hospital leverages smart automation to triage patients and prioritize urgent cases. Teams also use AI algorithms for image analysis and augmented reality for knowledge transfer. During surgeries, doctors can request instant peer advice via an AR platform. IoT-powered remote monitoring systems aid in follow-up care.
Greater adoption of remote patient care solutions reduced long waiting times and accelerated treatment start, leading to higher patient engagement and satisfaction. For healthcare practitioners, these systems reduce administrative toil and cost waste.
3. Data-Driven Senior Care Solutions
Rapid population aging is straining national healthcare systems.
OECD countries spend 1.5% of their gross domestic product on long-term care services like medical, nursing, personal, and assistance care. In Scandinavia and the Netherlands, spending is as high as 3.5% of GDP.
In the US, people over 55 account for 56% of total health spending, despite being only 30% of the population. Digital transformation in this area holds great promise for extending life, improving quality of life, and reducing the economic burdens of supporting senior citizens.
CarePredict launched a specialized wearable device for elderly care facilities. Wrist-worn, Tempo uses kinematic algorithms to process data and detect activities like eating, sleeping, and moving. It helps remotely ensure the elder’s healthy lifestyle without 24/7 camera monitoring. The platform also provides caretakers with biomarkers predictive of health declines like falls, UTIs, depression, or nutrition deficits.
CareZone, in turn, built an intuitive medication management app for senior citizens and their caregivers. The app allows users to create a comprehensive list of medications, set reminders, track history, and order refills in one click. Users can also scan the bottles to share prescriptions with doctors for faster refills.
Digital therapeutics programs for senior mental support have gained traction, showing promising outcomes in reducing cognitive decline and mental illness symptoms. Mynd developed a VR platform for engaging seniors in therapies that foster physical, cognitive, and mental wellness. Adopted at 15 skilled nursing facilities in Indiana, Mynd program had an 88% success in reducing feelings of isolation and increased socialization by 88% among participants.
Digital technologies enable caregivers to focus on the most important aspects of care and communication. With real-time data collection, centralized access, and robust analytics, they can continuously monitor patients’ well-being, ensure timely interventions, and optimize workloads.
4. Integration of AI into Healthcare Workflows
Machine learning (ML) and deep learning (DL), known as artificial intelligence (AI), are hot topics in healthcare. Skeptics worry about limited human interaction in the doctor-patient relationship, patient data privacy, and potential biases in automated systems.
Indeed, ML and DL systems cannot (and should not) fully replace human judgment. However, they are providing a massive aid for diagnostic support. Specialized medical image analysis models with AI have proven their capability for early disease detection, more accurate diagnoses, and streamlined surgical planning.
DeepMind AI for Radiography, which automatically detects and segments anatomical structures in chest X-rays, delivered 25% fewer false positives in a large mammography dataset, compared with commonly used clinical workflows – without missing any true positives.
AIR Recon DL — an MR image reconstruction solution from the GE Healthcare Edison platform — has benefited over two million patients globally. It increases MR image sharpness for a more confident diagnosis and reduces exam times by up to 50%.
Likewise, AI systems have excelled in health risk prediction and prevention, using patient data for providers to deliver appropriate interventions.
Mass General Hospital in the US has deployed AI models to predict surgical risk and determine the best interventions for high-risk patients. For example, TOP is an AI-powered app for predicting outcomes for trauma and emergency surgery patients. It’s instantly accessible, saving healthcare personnel time in decision-making.
Klarity, a HealthTech startup, built advanced models for predicting premature morbidity and chronic disease. Trained on a dataset of 634 million, the models use AI and expert-consensus-driven algorithms to deliver maximum outcome certainty. It can adapt to predict any medical risk by processing self-reported and wearable device data.
Beyond treatment support, AI systems can significantly aid with admin work, which takes up over 15% of physicians’ time on average. Generative AI, in particular, can streamline note-keeping, transcription, and recommendation-generation tasks.
A recent study found that 45% of medical summaries generated by LLMs were equivalent and 36% were superior to those from healthcare professionals. Additionally, the large language model summaries scored higher on conciseness, correctness, and completeness than the expert summaries.
In the US, companies like Abridge, Suki, and Microsoft’s Nuance are already successfully deploying gen AI for medical record management. Abridge automatically transforms patient conversations into digital notes with high accuracy. After adoption, Reid Health, achieved an 87% decrease in patient call turnaround time and a 60% decrease in after-hours documentation.
Suki offers more than note generation. It also does dictation, recommends medical codes, and incorporates live data, like patient vitals, from the EHR. According to the company, its assistant helps clinicians complete notes 72% faster and decreases amended encounter rates by 48%.
Overall, 83% of healthcare professionals believe that AI can eventually reduce many of the problems facing healthcare, especially in the areas of workflow efficiency, administration, and document management.
However, to profit from AI capabilities (and other emerging technologies), healthcare organizations will first need to resolve some of the remaining technical blockers.
How Leaders Approach Digital Transformations in Healthcare
Although digital transformation ambitions run high, progress often remains slow. Healthcare leaders cite “legacy systems”, “budget limitations”, “poor data quality”, and “inability to recruit top tech talent” as the main barriers.
The optimal approach to solving these challenges is partnerships with technology companies to develop or license new technologies.
Over 34 collaborations between Big Tech companies (Alphabet, Amazon, Microsoft, IBM) and healthcare institutions have been established as of 2023. In many cases, these include joint projects in adopting the company’s cloud services. Although some also have a synergistic relationship. For example, the Moorfields Eye Hospital in the UK, for example, provided DeepMind Health (part of Alphabet) a dataset of retina scans for training an AI model. In exchange, Moorfields can use DeepMind’s trained AI model to identify potentially blinding eye diseases
At the same time, many companies are also hiring software development partners to assist in digital transformation projects. According to Black Book Market Research, 93% of hospital leaders are employing more third-party vendors to implement digital technologies. manage IT infrastructure, maintain help desk functions, and handle big data management.
Strategic partnerships with software development companies can reallocate more resources towards patient-centric priorities, rather than IT function management. In addition, partnerships allow to circumnavigate ongoing technical staffing challenges and accelerate time-to-market for new initiatives.
For the last decade, Edvanits has been supporting healthcare businesses in their digital transformation efforts. We’ve helped launch a new telemedicine platform, now serving over a million patients, several remote prescription tools, and a range of advanced big data analytics solutions for healthcare. Contact us to learn more about our software engineering services.






