We’ve eliminated some of the most acute infections, but chronic diseases are now a growing problem. Globally, approximately one in three adults suffer from multiple chronic conditions (MCCs), and even more remain undiagnosed.
Due to labor shortages, healthcare systems struggle with an influx of patients needing regular check-ups and treatment plan adjustments. Chronic disease management is also expensive: 90% of US healthcare expenditures are spent treating these conditions.
Chronic diseases are preventable, but their prevalence is rising. By 2050, there will be 142.66 million people with at least one chronic disease, a 99.5% increase from 71.522 million in 2020.
Clearly, new approaches are required, and progressive healthcare organizations are considering chronic disease management software as a solution.
Why Chronic Disease Management Technology is In Demand
Many chronic diseases are lifestyle-related, caused by poor diet, lack of exercise, and excessive drinking. Historically, however, healthcare has focused on curative medicine (i.e., treatment of an exciting condition) rather than preventive medicine (i.e., averting a disease).
The sentiment, however, is changing. Global governments and healthcare organizations are focusing on preventive care to reduce escalating healthcare costs and prolong population longevity.
The Healthy People 2030 program in the US focuses on increasing access to preventive care for people of all ages. The European Society of Preventive Medicine (ESPM), a not-for-profit organization, facilitates research and advancements in preventive, predictive, and personalized medicine. Among EU Member States, spending on preventive healthcare is between 1%-5.6% of the total healthcare expenditure — and many countries seek to increase this proportion.
Patients who can’t regularly visit their healthcare provider unknowingly worsen their conditions. Low engagement results in missed intervention opportunities and faster disease progression, leading to worse health outcomes and higher healthcare costs.
However, physicians struggle to collect reliable patient data for treatment. They require better preventive and chronic disease management solutions to service large patient populations, ensure ongoing monitoring and engagement. This is critical for providers in traditional fee-for-service (FFS) agreements, and even more so for those participating in value-based care and risk-sharing agreements.
Until recently, implementing preventive medicine at scale was difficult as such programs required an increased staff count and more physical facilities. New healthcare technologies like cloud computing, big data analytics, and wearable devices are substantially improving the accessibility, speed, and efficiency of preventive healthcare delivery.
Nearly 3 in 5 physicians believe technology can be the most helpful in key areas such as chronic disease patients and preventative care.
American Medical Association
In the US, findings from Agency for Healthcare Research and Quality (AHRQ) funded projects provide evidence of improving chronic care and disease management using software and connected medical devices.
A study in three states found that remote monitoring of patients with congestive heart failure (CHF) can substantially reduce hospitalizations and ER trips. Patients used in-home devices to transmit health data like blood pressure and weight to a clinical decision support system. When significant changes were detected, both patients and healthcare providers were notified, leading to cost savings and improved patient confidence in managing their condition.
In Australia, more hospitals are partnering with companies to offer telemedicine, remote monitoring, and digital health platforms. Telstra Health, a digital healthcare platform, has signed over 540 hospitals in Australia. Their latest joint study with Mackay Hospital in Queensland found that virtual technology reduced 28-day hospital readmissions by 43% and shortened the average stay from 7.2 to 4 days, saving the health provider $3,698 per admission.
Eighty-six percent of executives in the healthcare sector acknowledge the potential cost reduction through digital health solutions.
EY Health Pulse Survey
Healthcare providers seek new ways to deliver better, faster, and cost-effective care. Digital healthcare technologies help free up hospital beds and ensure better patient outcomes. There’s a growing demand for better software in the chronic disease management market and under-serviced niches for new entrants.
6 Examples of Innovative Chronic Disease Management Software
Over 90% of healthcare organizations have adopted digital health strategies and are expanding their capabilities to develop high-precision care. Below are six particularly promising types of chronic disease management software solutions patients and hospitals seek to adopt.
Clinical Decision Support Systems (CDSS)
In 1950, medical knowledge doubled every 50 years—in 2021, it doubled every 73 days. More data leads to better clinical decision-making. Yet, healthcare providers struggle to assemble complete medical histories due to incomplete records, poor formatting, and extended patient history procurement time.
Clinical decision support systems (CDSS) increase the availability of patient records, such as allergies, symptoms, and medical history. As an information management tool, a CDSS applies big data analytics to electronic health records to provide suggestions to the healthcare provider. It processes data from remote patient monitoring systems, medical wearable devices, and historical records to provide comprehensive guidance.
Overview of the clinical decision support systems (CDSS) architecture
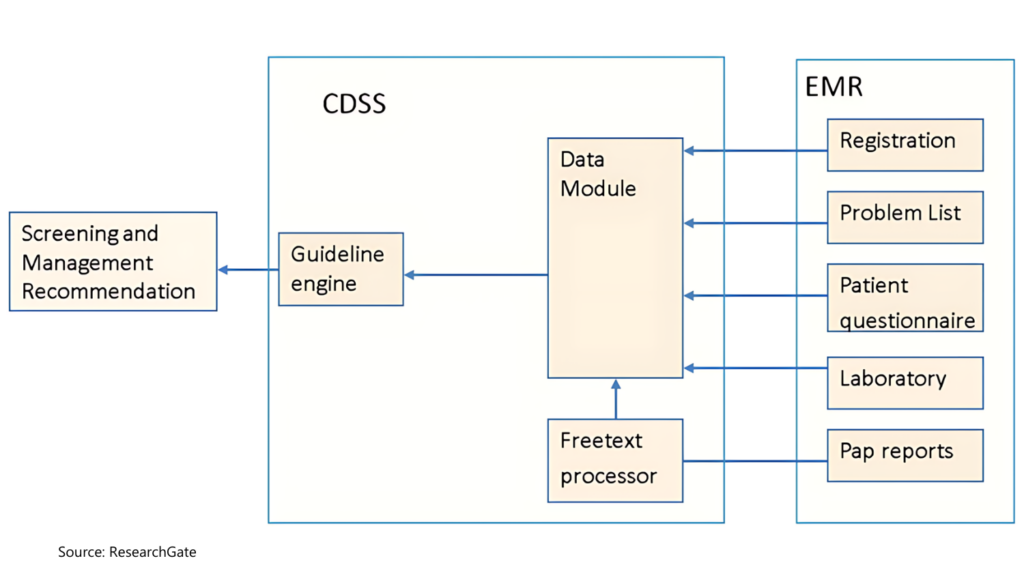
Source: ResearchGate
Modern solutions also include natural language processing (NLP) to integrate unstructured data (handwritten memos, medical images, audio notes) into decision-making. They also incorporate predictive analytics using machine learning (ML) to predict disease progression, complications, and administer preventive treatment. ML can detect unrecognized patterns in large data, accelerating clinical research and knowledge about diseases.
CDSS personalizes care by providing practitioners with data on the patient’s unique genetic, environmental, and lifestyle factors, as well as past treatment strategies. Over 40% of US hospitals already have advanced CDS capabilities, and common use cases include:
- Cardiovascular risk evaluation and management
- Diabetes medication prescribing and condition management
- Chronic kidney disease screening and management
Synapxe, Singapore’s HealthTech agency, recently presented a new national CDSS system for chronic disease management. Powered by a deep learning algorithm, the tool can identify risk factors, automate risk calculations, and detect early signs of various chronic diseases.
By improving healthcare data flows between various participants in the healthcare ecosystem, providers can offer holistic care efficiently, grounded in evidence.
Digital Therapeutics
Digital therapeutics (DX) is a rapidly growing domain of patient-facing software and hardware for remote interventions. Funding for DX projects increased by 133% between 2020 and 2021, reaching $3.4 billion.
DX solutions, like health wearables, mobile apps, and medical IoT devices, enable remote access to clinically proven treatment, improve adherence to medication, and allow personalized treatment.
For example, Fitterfly developed a digital chronic disease self-management program for diabetic patients. The app aggregates insights from different lab tests and the patients’ CGM to offer personalized guidance on nutrition, fitness, sleep, and stress management. Patients can access coaching or share their data with the healthcare provider. Clinical trials showed within 90 days, 46.9% of participants had HbA1c reduction of above 1%, and 38.5% had weight loss of above 4%.
Otsuka Pharmaceuticals and Click Therapeutics, in turn, just got FDA approval for their app-based digital therapeutic for major depressive disorder (MDD). The remote treatment program aims to improve patient emotion control through clinically-validated cognitive and emotional training, and short therapeutic exercises.
Countries globally are establishing regulatory frameworks for digital therapeutics products. Germany and the UK have included DTx products in reimbursement schemes. Interest and adoption rates are expected to accelerate in the coming years.
At-Home Care Systems
At the height of the global pandemic, Johns Hopkins Schools of Medicine and Public Health pioneered the Hospital at Home® program to provide hospital-level care in a patient’s home using remote healthcare. Over 100 healthcare facilities have implemented and continue to run this program well after the pandemic.
At-home acute care is an effective substitute for hospitalizations and frequent follow-up visits for short-term and long-term conditions. Remote patient monitoring and telehealth platforms allow practitioners to monitor vitals like blood glucose, pressure, and weight and provide care instructions via an app. Patients can report their qualitative symptoms, providing more data for decision-making. These insights can be streamed to a CDSS for further analysis and reference.
Mass General Brigham, an early adopter of at-home care, conducted a study among heart failure, chronic obstructive pulmonary disease, cancer, and dementia patients. At-home patients had fewer readmissions, fewer adverse events, and higher life expectancy.
UMass Memorial Health established an at-home care program to improve health equity among underserved populations. In the first two years, the number of patients transferring to nursing homes fell by 80%-90%, and health outcomes improved substantially.
The hospital-at-home market is expected to grow by 50% in the next five years as more hospitals join the program, encouraged by their peers’ positive results. This makes it another promising niche for HealthTech product development.
Virtual Nursing Platforms
Nursing staff shortages are significant in most markets and more professionals plan to leave. In a 2023 survey by McKinsey, 31% said they’re likely to leave direct patient care this year. The UK government aimed to recruit 500,000 extra nurses by 2024 but only hired 350,000 as of March 2024.
Virtual nursing platforms emerged as an innovative model to address ongoing staff shortages. As a form of telehealth, they provide hospitals with ‘on-call’ remote staff for tasks that don’t require physical proximity, like providing care instructions and patient education.
A pilot project with cancer outpatients found that combining remote patient management platforms and engaging patients daily with virtual nurses substantially improved patient outcomes. Results included 80% wearable device adherence and 100% blood pressure reading compliance achieved by 98.8%.
For chronic disease management, remote nurses are the primary point of contact, providing support and education to patients who cannot make frequent hospital visits. For example, the northern province of Nunavut in Canada launched a virtual nursing project to support its Chronic Disease Program. Virtual Nurse Practitioners (NPS) helped schedule screenings for chronic diseases or cancer among underserved populations, as well as ongoing monitoring. Since the start of the program, 90% of patients became up-to-date after their first intake appointment. The majority (97%) of patients with chronic diseases saw a positive change in their quality of life.
Moreover, 93% of patients reported receiving the same care quality with the virtual NP as in-person, and 94% feel their chronic disease was better managed through virtual visits.
Digital technologies aren’t just popular with patients. A 2023 study found that registered and licensed practical nurses have a higher acceptance of digital technologies than primary care providers (like physicians). They also prefer using technologies for case management and promoting healthy behaviors among patients.
Chronic Disease Management Apps
Dealing with a chronic disease is mentally taxing, especially without regular access to a ‘support network’ — like a friendly nurse or peers with similar symptoms. Chronic disease management apps provide a new medium for self-management and patient engagement. Patients can log symptoms, track medicine adherence, and receive personalized tips. Combined with medical wearable devices, apps obtain real-time health data and provide high-fidelity data to medical practitioners.
Effectively, a convenient app can help practitioners deliver personalized chronic disease management programs for a wider range of conditions via analytics-based advice on symptom management, regiment adjustment, and medication adherence.
For example, Hashiona mobile app offers a 20-week, step-by-step program to manage the well-being of Hashimoto’s patients with advice on stress management, exercise, and diet, as well as direct access to teleconsultations with specialists. Rune Labs, developed an advanced app to track symptoms of Parkinson’s disease, using patients’ neurology data.
Patients with chronic illness are also adjusting commercial wearable devices like Apple Watch and Fitbit to collect more personal data about their health trends and detect early warning signs. Clearly, there’s a strong demand for better symptom tracker apps for chronic disease.
VR Care Programs
Virtual reality (VR) is an emerging treatment that may reduce the negative effects of chronic physical illness and improve patients’ quality of life. Current technology already allows the creation of immersive experiences that closely mimic real-world therapy sessions.
In the UK, the largest-ever clinical trial of virtual reality (VR) therapy showed strong results for patients with psychosis. The gameChange VR program, developed by researchers at the University of Oxford and Oxford Health NHS Foundation Trust, targets the biggest fears psychosis patients experience: fears about being outside in everyday situations. With a VR headset, such patients don’t have to experience the extra stress of traveling to an appointment and progressively re-engage with day-to-day activities through virtual simulations and role-play.
AppliedVR, in turn, conducted a major clinical study of using VR for treating chronic low back pain. The research compared brain activation patterns and physiological metrics before, during, and after VR experiences among participants. Some were in a sham VR group and others received actual treatment from the RelieVRx medical device, which they used in combination with Kernel’s brain imaging headset. Participants of the RelieVRx program achieved a reduction in pain intensity by an average of 2.0 points and reported reductions in pain interference by 2.3 points, on average.
Apart from delivering direct interventions, the RelieVRx medical device also helps measure brain activation patterns and physiological metrics of patients. It helps clinicians better understand the patient’s symptoms and measure the efficacy of treatments. This can help develop more personalized treatment protocols and improve health outcomes.
Another digital therapeutic startup, XRHealth, works on combining medical extended reality (XR) technology with advanced data analytics on its platform to help clinicians treat patients with a broad range of chronic conditions like chronic pain, fibromyalgia, anxiety, stress, and dementia.
Final Thoughts
An increasing number of healthcare executives recognize the benefits digital health technologies bring to their organization: reduced readmissions, higher staff efficiency, better patient outcomes, and bottom-line growth
Chronic disease management software appears to be the next investment leaders want to implement to support their care programs. If you’re looking to enter into this market vertical, Edvantis healthcare software development team is here to assist. As experts in digitalization and big data analytics, we help global organizations launch convenient, secure, and scalable products to improve healthcare delivery and patient outcomes. Contact us to learn more about our services.


